Research progress on biomass and biomass-related hemostatic materials
-
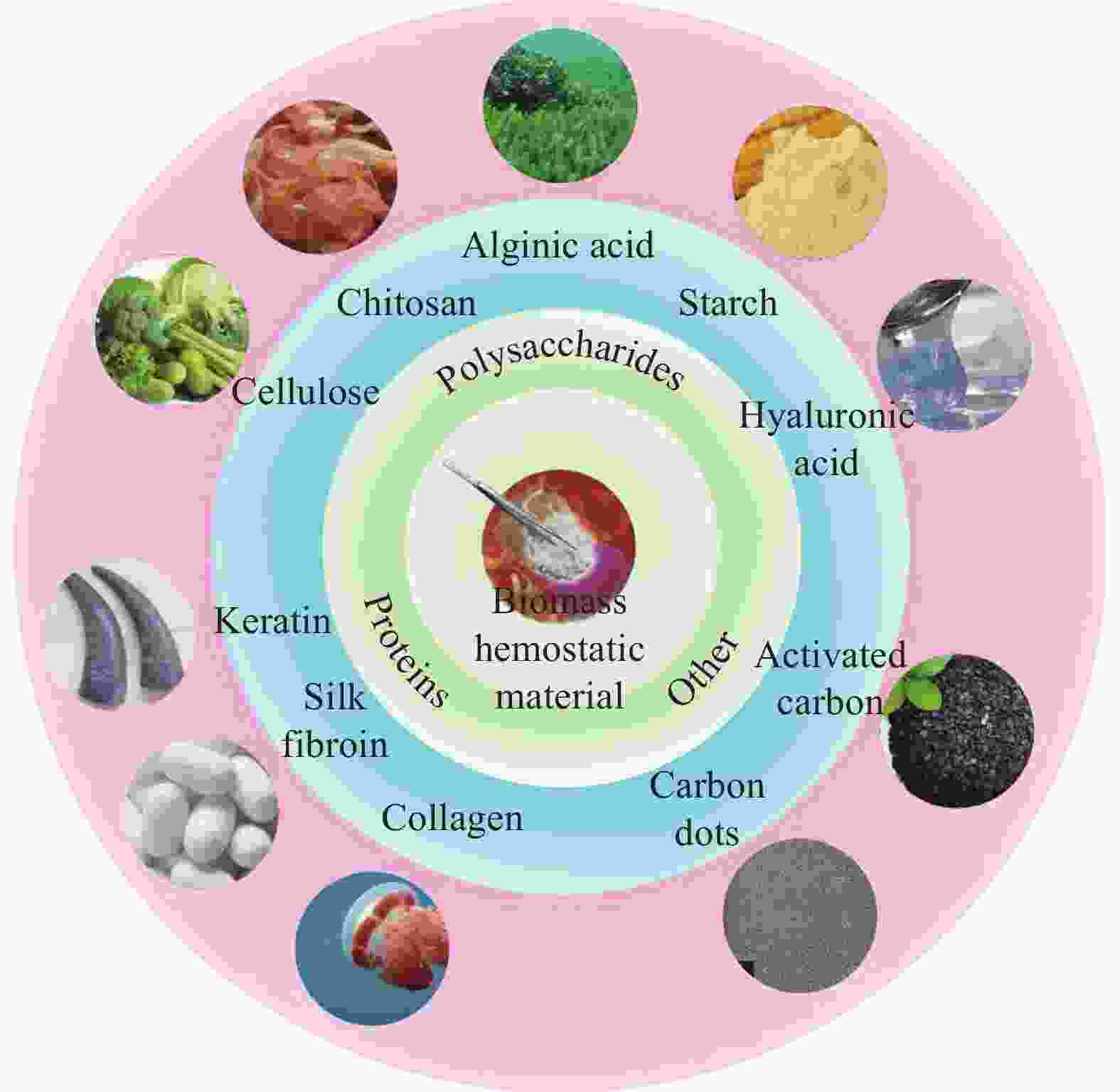
摘要: 伤口的快速止血和愈合对于解决意外事故造成的出血具有重要意义,相关止血材料的开发和应用一直备受关注。以角蛋白、丝素蛋白、胶原蛋白为代表的蛋白类和以纤维素、壳聚糖、海藻酸为代表的多糖类等生物质材料,因其无毒性、低抗原性、良好的生物相容性、生物可降解性等优点在止血领域展现了前所未有的应用价值。基于此,本文对生物质止血材料的设计、制备及止血应用的最新研究进展进行了全面综述,并对其发展前景做了展望,以期为新型高效止血材料的开发和实际应用提供思路。Abstract: The rapid hemostasis and healing of wounds after trauma hold great significance to solve the bleeding caused by accidents. Therefore, the development and application of related hemostatic materials have attracted much attention. Biomass-derived materials such as proteins including keratin, silk fibroin, collagen and polysaccharides including cellulose, chitosan, and alginic acid are favored by researchers because of their non-toxicity, low antigenicity, good biocompatibility, and biodegradability, and have shown unprecedented application value in the field of hemostasis. In this paper, the latest research results on the design, the preparation and the application of biomass hemostatic materials are comprehensively reviewed, and their development prospects are prospected, which will provide ideas for the development and practical application of new high-efficiency hemostatic materials.
-
Key words:
- biomass materials /
- protein /
- polysaccharide /
- hemostasis properties /
- wound hemostasis
-
图 2 (a) 截尾后给予SF-BGE、SFBGE/TA和SF-BGE/TA/ZnO水凝胶后失血的照片。(b) 对照组、SF-BGE、SF-BGE/TA、SF-BGE/TA、SF-BGE/TA/氧化锌水凝胶致伤大鼠的失血量 (Mg)。结果报告为平均值±标准差 (n=3)。统计学处理采用单因素方差分析和Tukey‘s后置检验 (*p < 0.05,**p < 0.01)。[48]
Figure 2. (a) Photographs of blood loss after tail amputation and administration of SF-BGE, SFBGE/TA and SF-BGE/TA/ZnO hydrogel. (b) Blood loss (mg) from injury rat tail of control, SF-BGE, SF-BGE/TA, and SF-BGE/TA/ZnO hydrogel. The results are reported as the mean ±standard deviation (n = 3). Statistical significance was analyzed by one-way ANOVA and Tukey’s post hoc test (* p < 0.05, ** p < 0.01).
图 4 (a) 大鼠断尾模型的止血时间。(b) 大鼠肝撕裂伤模型止血时间。(c) 大鼠断尾和肝撕裂模型的数字图像。将CSMS-K3涂于 (A) 尾部切割处和 (B) 肝撕裂伤处;涂抹CSMS-K3 5 min后 (C) 大鼠尾部切割处和 (D) 肝撕裂伤处。伤处形成暗红色血块,出血停止。[85]
Figure 4. (a) Hemostasis time in rat tail amputation model. (b) Hemostasis time in rat liver laceration model. (c) Digital images of rat tail amputation and liver laceration models. CSMS-K3 was applied onto (A) the tail cut and (B) on the liver injury; 5 min after application on the (C) rat tail cut and (D) the liver laceration. Dark-red blood clot was formed on the injured sites, bleeding stopped.[85]
图 5 纯海藻酸微球、Alg/Ag NPs、PGA/Alg/Ag NPs和PGA/Alg复合微球的止血分析。(a). 血浆凝血性能,(b). 凝血时间,(c). 凝血图像,(d). PGA/Alg/AgNPs微球的止血示意图
注:图5d (1) 止血剂提供外源性凝血成分,加速伤口血液凝结;(2) 止血剂促进红细胞、凝血因子、血小板聚集,加速凝血;(3) 止血剂吸收血液中水分,增加血细胞、血小板、凝血因子浓度,阻断创面,促进聚集止血。[93]
Figure 5. Hemostasis assays of pure alginate microspheres, Alg/Ag NPs, PGA/Alg/Ag NPs, and PGA/Alg composite microspheres. (a). blood plasma clotting performance, (b). clotting blood time, (c). coagulation images, (d). Schematic hemostasis of PGA/Alg/Ag NPs microspheres
Note: in Fig 5d (1) The hemostatic agent provides extrinsic coagulation components to accelerate blood clotting on the wound, (2) The hemostatic agent promotes the aggregation of red blood cells, coagulation factors and platelets, and accelerates the coagulation, (3) The hemostatic agent absorbs water in the blood, increases the concentration of blood cells, platelets, and coagulation factors, block the wound area and promotes the aggregation and hemostasis.[93]
表 1 现有商品化生物质止血材料
Table 1. Existing commercial biomass hemostatic materials
Hemostatic material Product name Manufacturer Mechanism of hemostasis Hemostatic effect Limitations or deficiencies References Fibrin sealant Tisseel Baxter Simulates the coagulation process in the body and quickly forms blood clots Complete hemostasis was achieved within 30 s (Arterial bypass) to 6 min (Carotid endarterectomy) The price is expensive, and the cost of transportation and storage is high; It is contraindicated in patients with bovine allergies, who have adverse effects including rash, coagulation disorders, anaphylaxis, and death from premade antibodies [16, 17] Evicel Ethicon Beriplast P CSL Behring Oxidized Cellulose Surgicel Johnson Immediately after the material encounters blood, the fluid in the blood is extracted and blood proteins, platelets, red blood cells and other active components are captured, resulting in an increased concentration of coagulation factors and an accelerated coagulation process Hemostasis is usually successful within 5 min (open surgery) Foreign body reactions, minor postoperative complications, as foci of infection or anaphylaxis, manifested mainly by acute dermatitis, eczema, and serous tumors [9, 18] Cutanplast B. Braun Surgicel Ethicon Gelatin Sponges Gelfoam Pfizer Attaches to the bleeding site, allowing platelets to stay in uniform pores, activating the coagulation cascade Hemostasis was successfully achieved within 5 min (reoperative cardiac surgery or emergency resternotomy) Inability to pack bleeding, and the possibility of breaking the clot when the sponge is removed; It may cause thrombosis of small blood vessels or an inflammatory reaction [17, 19]
Gelfoam
BaxterMicroporous Polysaccharides Arista AH Starch Medical It concentrates blood solids by absorbing water and low-molecular-weight compounds from the blood, thereby providing hemostasis and providing a scaffold for the formation of fibrin clots Haemostasis was completed at 1 min30 s (5 mm pork kidney incision) to 3 min20 s (12 mm pork kidney incision). There will be a slight inflammatory reaction at the beginning of use [20-22] Chitosan sponge HemCon HemCon Medical Technologies Positively charged chitosan binds to negatively charged red blood cells. As a result, it leads to the formation of sticky clots to promote hemostasis Complete hemostasis usually occurs within 2 min (Tooth extraction surgery) For limb injuries, tourniquets are required [23, 24] ChitoGauze PRO HemCon Medical Technologies Celox Z-Medica 表 2 蛋白类止血材料的材料类型、体内模型和止血效果
Table 2. Material types, in vivo models, and hemostatic effects of protein-based hemostatic materials
Hemostatic material Type of material Model of hemostasis Hemostatic effect Keratin Injectable hydrogel[34] Mouse model of liver injury Occlusion hemostasis was achieved in 90 s Nanoparticles[35] Rat model of liver injury and tail docking The hemostasis time was 60 s and 90 s Silk fibroin Composite sponge[47] Mouse model of liver injury 2 min 30 s to completely stop bleeding Nanocomposite hydrogels[48] Rat tail docking model The blood loss was only 183.4 ± 50.1 mg Collagen Porous sponges[56] Rat tail docking model Complete hemostasis in 5 min 20 s Nanofiber membranes[57] Rabbit ear artery, liver injury model The hemostasis time was 95.34 ± 10.05 s and 67.05 ± 7.15 s Self-healing hydrogel[58] Mouse hemorrhagic liver model The blood loss was only 0.4 ± 0.15 g 表 3 多糖类止血材料的材料类型、体内模型和止血效果
Table 3. Material types, in vivo models, and hemostatic effects of polysaccharide hemostatic materials
Hemostatic material Type of material Model of hemostasis Hemostatic effect Cellulose Composite sponge [67] Rat tail docking and liver injury model The blood loss was 159.46 mg and 80.44 mg Nanocomposite fibers [70] Lemonified human plasma, lemonified bovine whole blood The coagulation time was 143 ± 19 s and 67 ± 5 s Chitosan Powder [83] Mouse tail docking model The hemostasis time was 158 s, and the blood loss was only 11.0 mg Composite microspheres [85] A model of tail docking and liver laceration in rats The hemostasis time is 134 s and 99 s Composite hydrogel [86] Rat model of liver injury and femoral artery injury The hemostasis time was 53 ± 3 s and 189 ± 9 s Alginic acid Composite porous microspheres [91] Rat model of liver laceration and tail breakage The hemostasis time was 73 ± 5 s and 134 ± 5 s Foam [94] Porcine liver injury model The hemostasis time is 5 min Starch Superabsorbent
hydrogel [101]Rat model of femoral artery injury The hemostasis time < 10 s Powder [103] Rabbit model of ear vein, dorsal, femoral artery, liver injury The hemostasis time was 52 s, 46 s, 122 s and 102 s Drug-loaded microporous powder [105] Rabbit ear artery, liver injury model The hemostasis time is 108 ± 5 s and 120 ± 6 s Hyaluronic acid Sponge [113] Mouse model of liver injury The hemostasis time was < 60 s, and the blood loss was only 23.2 mg Cryogel [114] Rat model of liver injury The hemostasis time is 72 s -
[1] VOS T, LIM S S, ABBAFATI C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019[J]. The Lancet, 2020, 396(10258): 1204-1222. doi: 10.1016/S0140-6736(20)30925-9 [2] BAYLIS J R, LEE M M, ST JOHN A E, et al. Topical tranexamic acid inhibits fibrinolysis more effectively when formulated with self-propelling particles[J]. J Thromb Haemost, 2019, 17(10): 1645-1654. doi: 10.1111/jth.14526 [3] LIU C, LIU X, LIU C, et al. A highly efficient, in situ wet-adhesive dextran derivative sponge for rapid hemostasis[J]. Biomaterials, 2019, 205: 23-37. doi: 10.1016/j.biomaterials.2019.03.016 [4] HICKMAN D A, PAWLOWSKI C L, SEKHON U D S, et al. Biomaterials and Advanced Technologies for Hemostatic Management of Bleeding[J]. Adv Mater, 2018, 30(4): 1700859. doi: 10.1002/adma.201700859 [5] HOLCOMB J B, STANSBURY L G, CHAMPION H R, et al. Understanding combat casualty care statistics[J]. J Trauma, 2006, 60(2): 397-401. doi: 10.1097/01.ta.0000203581.75241.f1 [6] ZHONG Y, HU H, MIN N, et al. Application and outlook of topical hemostatic materials: a narrative review[J]. Ann Transl Med, 2021, 9(7): 577. doi: 10.21037/atm-20-7160 [7] GIDAY S A, KIM Y, KRISHNAMURTY D M, et al. Long-term randomized controlled trial of a novel nanopowder hemostatic agent (TC-325) for control of severe arterial upper gastrointestinal bleeding in a porcine model[J]. Endoscopy, 2011, 43(4): 296-299. doi: 10.1055/s-0030-1256125 [8] KATSUYAMA S, MIYAZAKI Y, KOBAYASHI S, et al. Novel, infection-free, advanced hemostatic material: physical properties and preclinical efficacy[J]. Minim Invasive Ther Allied Technol, 2020, 29(5): 283-292. doi: 10.1080/13645706.2019.1627373 [9] ZHANG S, LI J, CHEN S, et al. Oxidized cellulose-based hemostatic materials[J]. Carbohydr Polym, 2020, 230: 115585. doi: 10.1016/j.carbpol.2019.115585 [10] MONTAZERIAN H, DAVOODI E, BAIDYA A, et al. Engineered Hemostatic Biomaterials for Sealing Wounds[J]. Chem Rev, 2022, 122(15): 12864-12903. doi: 10.1021/acs.chemrev.1c01015 [11] YANG X, LIU W, LI N, et al. Design and development of polysaccharide hemostatic materials and their hemostatic mechanism[J]. Biomater Sci, 2017, 5(12): 2357-2368. doi: 10.1039/C7BM00554G [12] CHEN J, CHENG W, CHEN S, et al. Urushiol-functionalized mesoporous silica nanoparticles and their self-assembly into a Janus membrane as a highly efficient hemostatic material[J]. Nanoscale, 2018, 10(48): 22818-22829. doi: 10.1039/C8NR05882B [13] OTROCKA-DOMAGALA I, JASTRZEBSKI P, ADAMIAK Z, et al. Safety of the long-term application of QuikClot Combat Gauze, ChitoGauze PRO and Celox Gauze in a femoral artery injury model in swine - a preliminary study[J]. Pol J Vet Sci, 2016, 19(2): 337-343. doi: 10.1515/pjvs-2016-0041 [14] SUN X, LI J, SHAO K, et al. A composite sponge based on alkylated chitosan and diatom-biosilica for rapid hemostasis[J]. Int J Biol Macromol, 2021, 182: 2097-2107. doi: 10.1016/j.ijbiomac.2021.05.123 [15] YU L, ZHANG H, XIAO L, et al. A Bio-Inorganic Hybrid Hemostatic Gauze for Effective Control of Fatal Emergency Hemorrhage in “Platinum Ten Minutes”[J]. ACS Applied Materials & Interfaces, 2022, 14(19): 21814-21821. [16] ALBALA D M. Fibrin sealants in clinical practice[J]. Cardiovasc Surg, 2003, 11 Suppl 1: 5-11. [17] HONG Y M, LOUGHLIN K R. The use of hemostatic agents and sealants in urology[J]. J Urol, 2006, 176(6 Pt 1): 2367-2374. [18] AL-ATTAR N, DE JONGE E, KOCHARIAN R, et al. Safety and Hemostatic Effectiveness of SURGICEL(R) Powder in Mild and Moderate Intraoperative Bleeding[J]. Clin Appl Thromb Hemost, 2023, 29: 10760296231190376. [19] KTARI O, FRASSANITO P, GESSI M, et al. Gelfoam Migration: A Potential Cause of Recurrent Hydrocephalus[J]. World Neurosurg, 2020, 142: 212-217. doi: 10.1016/j.wneu.2020.06.214 [20] HUMPHREYS M R, LINGEMAN J E, TERRY C, et al. Renal injury and the application of polysaccharide hemospheres: a laparoscopic experimental model[J]. J Endourol, 2008, 22(6): 1375-1381. doi: 10.1089/end.2008.0008 [21] LYBARGER K S. Review of Evidence Supporting the Arista Absorbable Powder Hemostat[J]. Med Devices (Auckl), 2024, 17: 173-188. [22] ZHU J, WU Z, SUN W, et al. Hemostatic Efficacy and Biocompatibility Evaluation of a Novel Absorbable Porous Starch Hemostat[J]. Surg Innov, 2022, 29(3): 367-377. doi: 10.1177/15533506211046100 [23] AZARGOON H, WILLIAMS B J, SOLOMON E S, et al. Assessment of hemostatic efficacy and osseous wound healing using HemCon dental dressing[J]. J Endod, 2011, 37(6): 807-811. doi: 10.1016/j.joen.2011.02.023 [24] WEDMORE I, MCMANUS J G, PUSATERI A E, et al. A special report on the chitosan-based hemostatic dressing: experience in current combat operations[J]. J Trauma, 2006, 60(3): 655-658. doi: 10.1097/01.ta.0000199392.91772.44 [25] BURNETT L R, RAHMANY M B, RICHTER J R, et al. Hemostatic properties and the role of cell receptor recognition in human hair keratin protein hydrogels[J]. Biomaterials, 2013, 34(11): 2632-2640. doi: 10.1016/j.biomaterials.2012.12.022 [26] LUSIANA, REICHL S, MULLER-GOYMANN C C. Keratin film made of human hair as a nail plate model for studying drug permeation[J]. Eur J Pharm Biopharm, 2011, 78(3): 432-440. doi: 10.1016/j.ejpb.2011.01.022 [27] SHAVANDI A, SILVA T H, BEKHIT A A, et al. Keratin: dissolution, extraction and biomedical application[J]. Biomater Sci, 2017, 5(9): 1699-1735. doi: 10.1039/C7BM00411G [28] YAN R R, XUE D, SU C, et al. A keratin/chitosan sponge with excellent hemostatic performance for uncontrolled bleeding[J]. Colloids and surfaces B, Biointerfaces, 2022, 218: 112770. doi: 10.1016/j.colsurfb.2022.112770 [29] YE W, QIN M, QIU R, et al. Keratin-based wound dressings: From waste to wealth[J]. Int J Biol Macromol, 2022, 211: 183-197. doi: 10.1016/j.ijbiomac.2022.04.216 [30] FENG C C, LU W F, LIU Y C, et al. A hemostatic keratin/alginate hydrogel scaffold with methylene blue mediated antimicrobial photodynamic therapy[J]. Journal of materials chemistry B, 2022, 10(25): 4878-4888. doi: 10.1039/D2TB00898J [31] VERMA V, VERMA P, RAY P, et al. Preparation of scaffolds from human hair proteins for tissue-engineering applications[J]. Biomed Mater, 2008, 3(2): 025007. doi: 10.1088/1748-6041/3/2/025007 [32] ABOUSHWAREB T, EBERLI D, WARD C, et al. A keratin biomaterial gel hemostat derived from human hair: evaluation in a rabbit model of lethal liver injury[J]. J Biomed Mater Res B Appl Biomater, 2009, 90(1): 45-54. [33] RAHMANY M B, HANTGAN R R, VAN DYKE M. A mechanistic investigation of the effect of keratin-based hemostatic agents on coagulation[J]. Biomaterials, 2013, 34(10): 2492-2500. doi: 10.1016/j.biomaterials.2012.12.008 [34] TANG A, LI Y, YAO Y, et al. Injectable keratin hydrogels as hemostatic and wound dressing materials[J]. Biomater Sci, 2021, 9(11): 4169-4177. doi: 10.1039/D1BM00135C [35] LUO T, HAO S, CHEN X, et al. Development and assessment of kerateine nanoparticles for use as a hemostatic agent[J]. Mater Sci Eng C Mater Biol Appl, 2016, 63: 352-358. doi: 10.1016/j.msec.2016.03.007 [36] HAGHNIAZ R, GANGRADE A, MONTAZERIAN H, et al. An All-In-One Transient Theranostic Platform for Intelligent Management of Hemorrhage[J]. Adv Sci (Weinh), 2023, 10(24): e2301406. doi: 10.1002/advs.202301406 [37] ZHU H, WU B, FENG X, et al. Preparation and characterization of bioactive mesoporous calcium silicate-silk fibroin composite films[J]. J Biomed Mater Res B Appl Biomater, 2011, 98(2): 330-341. [38] SARAN K, SHI P, RANJAN S, et al. A moldable putty containing silk fibroin yolk shell particles for improved hemostasis and bone repair[J]. Adv Healthc Mater, 2015, 4(3): 432-445. doi: 10.1002/adhm.201400411 [39] WEI W, LIU J, PENG Z, et al. Gellable silk fibroin-polyethylene sponge for hemostasis[J]. Artif Cells Nanomed Biotechnol, 2020, 48(1): 28-36. doi: 10.1080/21691401.2019.1699805 [40] GIL E S, PANILAITIS B, BELLAS E, et al. Functionalized silk biomaterials for wound healing[J]. Adv Healthc Mater, 2013, 2(1): 206-217. doi: 10.1002/adhm.201200192 [41] LI X, LI B, MA J, et al. Development of a silk fibroin/HTCC/PVA sponge for chronic wound dressing[J]. Journal of Bioactive and Compatible Polymers, 2014, 29(4): 398-411. doi: 10.1177/0883911514537731 [42] QIAO Z, LV X, HE S, et al. A mussel-inspired supramolecular hydrogel with robust tissue anchor for rapid hemostasis of arterial and visceral bleedings[J]. Bioact Mater, 2021, 6(9): 2829-2840. [43] SHEFA A A, TAZ M, LEE S Y, et al. Enhancement of hemostatic property of plant derived oxidized nanocellulose-silk fibroin based scaffolds by thrombin loading[J]. Carbohydr Polym, 2019, 208: 168-179. doi: 10.1016/j.carbpol.2018.12.056 [44] LEI C, ZHU H, LI J, et al. Preparation and hemostatic property of low molecular weight silk fibroin[J]. J Biomater Sci Polym Ed, 2016, 27(5): 403-418. doi: 10.1080/09205063.2015.1136918 [45] BARKUN A N, MOOSAVI S, MARTEL M. Topical hemostatic agents: a systematic review with particular emphasis on endoscopic application in GI bleeding[J]. Gastrointest Endosc, 2013, 77(5): 692-700. doi: 10.1016/j.gie.2013.01.020 [46] HUANG X, FU Q, DENG Y, et al. Surface roughness of silk fibroin/alginate microspheres for rapid hemostasis in vitro and in vivo[J]. Carbohydr Polym, 2021, 253: 117256. doi: 10.1016/j.carbpol.2020.117256 [47] LEE J, CHOI H N, CHA H J, et al. Microporous Hemostatic Sponge Based on Silk Fibroin and Starch with Increased Structural Retentivity for Contact Activation of the Coagulation Cascade[J]. Biomacromolecules, 2023, 24(4): 1763-1773. doi: 10.1021/acs.biomac.2c01512 [48] YANG C M, LEE J, LEE S Y, et al. Silk Fibroin/Tannin/ZnO Nanocomposite Hydrogel with Hemostatic Activities[J]. Gels, 2022, 8(10): 650. doi: 10.3390/gels8100650 [49] SUN L, LI B, SONG W, et al. Comprehensive assessment of Nile tilapia skin collagen sponges as hemostatic dressings[J]. Materials Science and Engineering: C, 2020, 109: 110532. doi: 10.1016/j.msec.2019.110532 [50] LIU X, ZHENG M, WANG X, et al. Biofabrication and Characterization of Collagens with Different Hierarchical Architectures[J]. ACS Biomaterials Science & Engineering, 2019, 6(1): 739-748. [51] JIANG X, WANG Y, FAN D, et al. A novel human-like collagen hemostatic sponge with uniform morphology, good biodegradability and biocompatibility[J]. Journal of Biomaterials Applications, 2017, 31(8): 1099-1107. doi: 10.1177/0885328216687663 [52] WANG Q, CHEN J, WANG D, et al. Rapid Hemostatic Biomaterial from a Natural Bath Sponge Skeleton[J]. Marine Drugs, 2021, 19(4): 220. doi: 10.3390/md19040220 [53] BROEKEMA F I, VAN OEVEREN W, BOERENDONK A, et al. Hemostatic action of polyurethane foam with 55% polyethylene glycol compared to collagen and gelatin[J]. Bio-Medical Materials and Engineering, 2016, 27(2-3): 149-159. doi: 10.3233/BME-161578 [54] LUO J, MENG Y, ZHENG L, et al. Fabrication and characterization of Chinese giant salamander skin composite collagen sponge as a high-strength rapid hemostatic material[J]. Journal of Biomaterials Science, Polymer Edition, 2018, 30(4): 247-262. [55] SHI X, FANG Q, DING M, et al. Microspheres of carboxymethyl chitosan, sodium alginate and collagen for a novel hemostatic in vitro study[J]. Journal of Biomaterials Applications, 2015, 30(7): 1092-1102. [56] DAO M, CHENG X, SHAO Z, et al. Isolation, Characterization and Evaluation of Collagen from Jellyfish Rhopilema esculentum Kishinouye for Use in Hemostatic Applications[J]. Plos One, 2017, 12(1): e0169731. doi: 10.1371/journal.pone.0169731 [57] CHENG W, ZHANG Z, XU R, et al. Incorporation of bacteriophages in polycaprolactone/collagen fibers for antibacterial hemostatic dual-function[J]. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 2018, 106(7): 2588-2595. doi: 10.1002/jbm.b.34075 [58] DING C, TIAN M, FENG R, et al. Novel Self-Healing Hydrogel with Injectable, pH-Responsive, Strain-Sensitive, Promoting Wound-Healing, and Hemostatic Properties Based on Collagen and Chitosan[J]. ACS Biomaterials Science & Engineering, 2020, 6(7): 3855-3867. [59] CIDREIRA A C M, DE CASTRO K C, HATAMI T, et al. Cellulose nanocrystals-based materials as hemostatic agents for wound dressings: a review[J]. Biomedical Microdevices, 2021, 23(4): 43. doi: 10.1007/s10544-021-00581-0 [60] FAN X, LI M, YANG Q, et al. Morphology-controllable cellulose/chitosan sponge for deep wound hemostasis with surfactant and pore-foaming agent[J]. Materials Science and Engineering: C, 2021, 118: 111408. doi: 10.1016/j.msec.2020.111408 [61] FAN X, LI Y, LI N, et al. Rapid hemostatic chitosan/cellulose composite sponge by alkali/urea method for massive haemorrhage[J]. International Journal of Biological Macromolecules, 2020, 164: 2769-2778. doi: 10.1016/j.ijbiomac.2020.07.312 [62] LAURENCE S, BAREILLE R, BAQUEY C, et al. Development of a resorbable macroporous cellulosic material used as hemostatic in an osseous environment[J]. Journal of Biomedical Materials Research Part A, 2005, 73A(4): 422-429. doi: 10.1002/jbm.a.30280 [63] LI B, PAN W, SUN X, et al. Hemostatic effect and safety evaluation of oxidized regenerated cellulose in total knee arthroplasty- a randomized controlledtrial[J]. BMC Musculoskeletal Disorders, 2023, 24(1): 797. doi: 10.1186/s12891-023-06932-7 [64] AYDEMIR SEZER U, SAHIN İ, ARU B, et al. Cytotoxicity, bactericidal and hemostatic evaluation of oxidized cellulose microparticles: Structure and oxidation degree approach[J]. Carbohydrate Polymers, 2019, 219: 87-94. doi: 10.1016/j.carbpol.2019.05.005 [65] HERNáNDEZ-BONILLA S, RODRíGUEZ-GARCíA A M, JIMéNEZ-HEFFERNAN J A, et al. FNA cytology of postoperative pseudotumoral lesions induced by oxidized cellulose hemostatic agents[J]. Cancer Cytopathology, 2019, 127(12): 765-770. doi: 10.1002/cncy.22194 [66] VELáZQUEZ-AVIñA J, MöNKEMüLLER K, SAKAI P, et al. Hemostatic effect of oxidized regenerated cellulose in an experimental gastric mucosal resection model[J]. Endoscopy, 2014, 46(10): 878-882. doi: 10.1055/s-0034-1365494 [67] BIAN J, BAO L, GAO X, et al. Bacteria-engineered porous sponge for hemostasis and vascularization[J]. Journal of Nanobiotechnology, 2022, 20(1): 47. doi: 10.1186/s12951-022-01254-7 [68] OHTA S, NISHIYAMA T, SAKODA M, et al. Development of carboxymethyl cellulose nonwoven sheet as a novel hemostatic agent[J]. Journal of Bioscience and Bioengineering, 2015, 119(6): 718-723. doi: 10.1016/j.jbiosc.2014.10.026 [69] LIU R, DAI L, SI C, et al. Antibacterial and hemostatic hydrogel via nanocomposite from cellulose nanofibers[J]. Carbohydrate Polymers, 2018, 195: 63-70. doi: 10.1016/j.carbpol.2018.04.085 [70] UDANGAWA R N, MIKAEL P E, MANCINELLI C, et al. Novel Cellulose–Halloysite Hemostatic Nanocomposite Fibers with a Dramatic Reduction in Human Plasma Coagulation Time[J]. ACS Applied Materials & Interfaces, 2019, 11(17): 15447-15456. [71] WU Z, ZHOU W, DENG W, et al. Antibacterial and Hemostatic Thiol-Modified Chitosan-Immobilized AgNPs Composite Sponges[J]. ACS Applied Materials & Interfaces, 2020, 12(18): 20307-20320. [72] RADWAN-PRAGŁOWSKA J, PIĄTKOWSKI M, DEINEKA V, et al. Chitosan-Based Bioactive Hemostatic Agents with Antibacterial Properties—Synthesis and Characterization[J]. Molecules, 2019, 24(14). [73] LAN G, LU B, WANG T, et al. Chitosan/gelatin composite sponge is an absorbable surgical hemostatic agent[J]. Colloids and Surfaces B: Biointerfaces, 2015, 136: 1026-1034. doi: 10.1016/j.colsurfb.2015.10.039 [74] GHEORGHIȚĂ D, MOLDOVAN H, ROBU A, et al. Chitosan-Based Biomaterials for Hemostatic Applications: A Review of Recent Advances[J]. International Journal of Molecular Sciences, 2023, 24(13): 10540. doi: 10.3390/ijms241310540 [75] HU Z, ZHANG D-Y, LU S-T, et al. Chitosan-Based Composite Materials for Prospective Hemostatic Applications[J]. Marine Drugs, 2018, 16(8): 273. doi: 10.3390/md16080273 [76] YAN T, CHENG F, WEI X, et al. Biodegradable collagen sponge reinforced with chitosan/calcium pyrophosphate nanoflowers for rapid hemostasis[J]. Carbohydrate Polymers, 2017, 170: 271-280. doi: 10.1016/j.carbpol.2017.04.080 [77] DOWLING M B, KUMAR R, KEIBLER M A, et al. A self-assembling hydrophobically modified chitosan capable of reversible hemostatic action[J]. Biomaterials, 2011, 32(13): 3351-3357. doi: 10.1016/j.biomaterials.2010.12.033 [78] KUMAR A, VIMAL A, KUMAR A. Why Chitosan? From properties to perspective of mucosal drug delivery[J]. International Journal of Biological Macromolecules, 2016, 91: 615-622. doi: 10.1016/j.ijbiomac.2016.05.054 [79] BELLICH B, D’AGOSTINO I, SEMERARO S, et al. “The Good, the Bad and the Ugly” of Chitosans[J]. Marine Drugs, 2016, 14(5): 99. doi: 10.3390/md14050099 [80] KHAN M A, MUJAHID M. A review on recent advances in chitosan based composite for hemostatic dressings[J]. International Journal of Biological Macromolecules, 2019, 124: 138-147. doi: 10.1016/j.ijbiomac.2018.11.045 [81] LORD M S, CHENG B, MCCARTHY S J, et al. The modulation of platelet adhesion and activation by chitosan through plasma and extracellular matrix proteins[J]. Biomaterials, 2011, 32(28): 6655-6662. doi: 10.1016/j.biomaterials.2011.05.062 [82] FISCHER T, THATTE H, NICHOLS T, et al. Synergistic platelet integrin signaling and factor XII activation in poly--acetyl glucosamine fiber-mediated hemostasis[J]. Biomaterials, 2005, 26(27): 5433-5443. [83] WU S, HUANG Z, YUE J, et al. The efficient hemostatic effect of Antarctic krill chitosan is related to its hydration property[J]. Carbohydrate Polymers, 2015, 132: 295-303. doi: 10.1016/j.carbpol.2015.06.030 [84] LI B, WANG J, GUI Q, et al. Continuous production of uniform chitosan beads as hemostatic dressings by a facile flow injection method[J]. Journal of Materials Chemistry B, 2020, 8(35): 7941-7946. doi: 10.1039/D0TB01462A [85] SUN X, TANG Z, PAN M, et al. Chitosan/kaolin composite porous microspheres with high hemostatic efficacy[J]. Carbohydrate Polymers, 2017, 177: 135-143. doi: 10.1016/j.carbpol.2017.08.131 [86] SUNDARAM M N, AMIRTHALINGAM S, MONY U, et al. Injectable chitosan-nano bioglass composite hemostatic hydrogel for effective bleeding control[J]. International Journal of Biological Macromolecules, 2019, 129: 936-943. doi: 10.1016/j.ijbiomac.2019.01.220 [87] ZHENG Y, PAN N, LIU Y, et al. Novel porous chitosan/N-halamine structure with efficient antibacterial and hemostatic properties[J]. Carbohydrate Polymers, 2021, 253: 117205. doi: 10.1016/j.carbpol.2020.117205 [88] LEE K Y, MOONEY D J. Alginate: Properties and biomedical applications[J]. Progress in Polymer Science, 2012, 37(1): 106-126. doi: 10.1016/j.progpolymsci.2011.06.003 [89] CHEN Y, WU L, LI P, et al. Polysaccharide Based Hemostatic Strategy for Ultrarapid Hemostasis[J]. Macromolecular Bioscience, 2020, 20(4): e1900370. doi: 10.1002/mabi.201900370 [90] ALAVI M, RAI M. Recent progress in nanoformulations of silver nanoparticles with cellulose, chitosan, and alginic acid biopolymers for antibacterial applications[J]. Applied Microbiology and Biotechnology, 2019, 103(21-22): 8669-8676. doi: 10.1007/s00253-019-10126-4 [91] PAN M, TANG Z, TU J, et al. Porous chitosan microspheres containing zinc ion for enhanced thrombosis and hemostasis[J]. Materials Science and Engineering: C, 2018, 85: 27-36. doi: 10.1016/j.msec.2017.12.015 [92] ZHONG W. Efficacy and toxicity of antibacterial agents used in wound dressings[J]. Cutaneous and ocular toxicology, 2015, 34(1): 61-67. doi: 10.3109/15569527.2014.890939 [93] TONG Z, YANG J, LIN L, et al. In situ synthesis of poly (γ- glutamic acid)/alginate/AgNP composite microspheres with antibacterial and hemostatic properties[J]. Carbohydrate Polymers, 2019, 221: 21-28. doi: 10.1016/j.carbpol.2019.05.035 [94] CHOUDHARY H, RUDY M B, DOWLING M B, et al. Foams with Enhanced Rheology for Stopping Bleeding[J]. ACS Applied Materials & Interfaces, 2021, 13(12): 13958-13967. [95] ZHENG Y, SHARIATI K, GHOVVATI M, et al. Hemostatic patch with ultra-strengthened mechanical properties for efficient adhesion to wet surfaces[J]. Biomaterials, 2023, 301: 122240. doi: 10.1016/j.biomaterials.2023.122240 [96] YANG X, LIU W, XI G, et al. Fabricating antimicrobial peptide-immobilized starch sponges for hemorrhage control and antibacterial treatment[J]. Carbohydrate Polymers, 2019, 222. [97] CHEN J, CHEN S, CHENG W, et al. Fabrication of porous starch microspheres by electrostatic spray and supercritical CO2 and its hemostatic performance[J]. International Journal of Biological Macromolecules, 2019, 123: 1-9. doi: 10.1016/j.ijbiomac.2018.10.219 [98] PAVLOVIC S, BRANDAO P R G. Adsorption of starch, amylose, amylopectin and glucose monomer and their effect on the flotation of hematite and quartz[J]. Minerals Engineering, 2003, 16(11): 1117-1122. doi: 10.1016/j.mineng.2003.06.011 [99] LIU G, GU Z, HONG Y, et al. Electrospun starch nanofibers: Recent advances, challenges, and strategies for potential pharmaceutical applications[J]. Journal of Controlled Release, 2017, 252: 95-107. doi: 10.1016/j.jconrel.2017.03.016 [100] CHEN F, CAO X, YU J, et al. Quaternary Ammonium Groups Modified Starch Microspheres for Instant Hemorrhage Control[J]. Colloids and Surfaces B: Biointerfaces, 2017, 159: 937-944. doi: 10.1016/j.colsurfb.2017.08.024 [101] MIRZAKHANIAN Z, FAGHIHI K, BARATI A, et al. Synthesis and characterization of fast-swelling porous superabsorbent hydrogel based on starch as a hemostatic agent[J]. Journal of Biomaterials Science, Polymer Edition, 2015, 26(18): 1439-1451. doi: 10.1080/09205063.2015.1100496 [102] AWASTHI G P, ADHIKARI S P, KO S, et al. Facile synthesis of ZnO flowers modified graphene like MoS2 sheets for enhanced visible-light-driven photocatalytic activity and antibacterial properties[J]. Journal of Alloys and Compounds, 2016, 682: 208-215. doi: 10.1016/j.jallcom.2016.04.267 [103] HOU Y, XIA Y, PAN Y, et al. Influences of mesoporous zinc-calcium silicate on water absorption, degradability, antibacterial efficacy, hemostatic performances and cell viability to microporous starch based hemostat[J]. Materials Science and Engineering: C, 2017, 76: 340-349. doi: 10.1016/j.msec.2017.03.094 [104] QIAN J, CHEN Y, YANG H, et al. Preparation and characterization of crosslinked porous starch hemostatic[J]. International Journal of Biological Macromolecules, 2020, 160: 429-436. doi: 10.1016/j.ijbiomac.2020.05.189 [105] SU H, WEI S, CHEN F, et al. Tranexamic acid-loaded starch hemostatic microspheres[J]. RSC Advances, 2019, 9(11): 6245-6253. doi: 10.1039/C8RA06662K [106] CUI R, CHEN F, ZHAO Y, et al. A novel injectable starch-based tissue adhesive for hemostasis[J]. Journal of Materials Chemistry B, 2020, 8(36): 8282-8293. doi: 10.1039/D0TB01562H [107] SU Y, CHEN H, LIU Q, et al. Thermoresponsive Gels with Embedded Starch Microspheres for Optimized Antibacterial and Hemostatic Properties[J]. ACS Applied Materials & Interfaces, 2024, 16(10): 12321-12331. [108] MASTERS K S, SHAH D N, LEINWAND L A, et al. Crosslinked hyaluronan scaffolds as a biologically active carrier for valvular interstitial cells[J]. Biomaterials, 2005, 26(15): 2517-2525. doi: 10.1016/j.biomaterials.2004.07.018 [109] YAMANLAR S, SANT S, BOUDOU T, et al. Surface functionalization of hyaluronic acid hydrogels by polyelectrolyte multilayer films[J]. Biomaterials, 2011, 32(24): 5590-5599. doi: 10.1016/j.biomaterials.2011.04.030 [110] WANG Y, LIU G, WU L, et al. Rational design of porous starch/hyaluronic acid composites for hemostasis[J]. International Journal of Biological Macromolecules, 2020, 158: 1319-1329. doi: 10.1016/j.ijbiomac.2020.05.018 [111] ABALLAY A, HERMANS M H E. Neodermis Formation in Full Thickness Wounds Using an Esterified Hyaluronic Acid Matrix[J]. J Burn Care Res, 2019, 40(5): 585-589. doi: 10.1093/jbcr/irz057 [112] ROEHRS H, STOCCO J G, POTT F, et al. Dressings and topical agents containing hyaluronic acid for chronic wound healing[J]. The Cochrane database of systematic reviews, 2023, 7(7): Cd012215. [113] LIU J-Y, LI Y, HU Y, et al. Hemostatic porous sponges of cross-linked hyaluronic acid/cationized dextran by one self-foaming process[J]. Materials Science and Engineering: C, 2018, 83: 160-168. doi: 10.1016/j.msec.2017.10.007 [114] WANG M, HU J, OU Y, et al. Shape-Recoverable Hyaluronic Acid–Waterborne Polyurethane Hybrid Cryogel Accelerates Hemostasis and Wound Healing[J]. ACS Applied Materials & Interfaces, 2022, 14(15): 17093-17108. [115] CHEN Z, YE S-Y, YANG Y, et al. A review on charred traditional Chinese herbs: carbonization to yield a haemostatic effect[J]. Pharmaceutical Biology, 2019, 57(1): 498-506. doi: 10.1080/13880209.2019.1645700 [116] DONG X, LIANG W, MEZIANI M J, et al. Carbon Dots as Potent Antimicrobial Agents[J]. Theranostics, 2020, 10(2): 671-686. doi: 10.7150/thno.39863 [117] LI D, XU K-Y, ZHAO W-P, et al. Chinese Medicinal Herb-Derived Carbon Dots for Common Diseases: Efficacies and Potential Mechanisms[J]. Frontiers in Pharmacology, 2022, 13. [118] SZCZEPANKOWSKA J, KHACHATRYAN G, KHACHATRYAN K, et al. Carbon Dots—Types, Obtaining and Application in Biotechnology and Food Technology[J]. International Journal of Molecular Sciences, 2023, 24(19). [119] VILLALBA-RODRíGUEZ A M, GONZáLEZ-GONZáLEZ R B, MARTíNEZ-RUIZ M, et al. Chitosan-Based Carbon Dots with Applied Aspects: New Frontiers of International Interest in a Material of Marine Origin[J]. Marine Drugs, 2022, 20(12): 782. doi: 10.3390/md20120782 [120] KRYSTYJAN M, KHACHATRYAN G, KHACHATRYAN K, et al. Polysaccharides Composite Materials as Carbon Nanoparticles Carrier[J]. Polymers, 2022, 14(5): 948. doi: 10.3390/polym14050948 [121] YAN X, ZHAO Y, LUO J, et al. Hemostatic bioactivity of novel Pollen Typhae Carbonisata-derived carbon quantum dots[J]. Journal of Nanobiotechnology, 2017, 15(1): 60. doi: 10.1186/s12951-017-0296-z [122] LI S, GUO Z, ZHANG Y, et al. Blood Compatibility Evaluations of Fluorescent Carbon Dots[J]. ACS Applied Materials & Interfaces, 2015, 7(34): 19153-19162. [123] HAN B, SHEN L, XIE H, et al. Synthesis of Carbon Dots with Hemostatic Effects Using Traditional Chinese Medicine as a Biomass Carbon Source[J]. ACS Omega, 2023, 8(3): 3176-3183. doi: 10.1021/acsomega.2c06600 [124] WU T, LI M, LI T, et al. Natural biomass-derived carbon dots as a potent solubilizer with high biocompatibility and enhanced antioxidant activity[J]. Front Mol Biosci, 2023, 10: 1284599. doi: 10.3389/fmolb.2023.1284599 [125] ZHANG J, ZOU L, LI Q, et al. Carbon Dots Derived from Traditional Chinese Medicines with Bioactivities: A Rising Star in Clinical Treatment[J]. ACS Appl Bio Mater, 2023, 6(10): 3984-4001. doi: 10.1021/acsabm.3c00462 [126] SUN Z, LU F, CHENG J, et al. Haemostatic bioactivity of novel Schizonepetae Spica Carbonisata-derived carbon dots via platelet counts elevation[J]. Artificial Cells, Nanomedicine, and Biotechnology, 2018, 46(sup3): 308-317. doi: 10.1080/21691401.2018.1492419 [127] LIU X, WANG Y, YAN X, et al. Novel Phellodendri Cortex (Huang Bo)-derived carbon dots and their hemostatic effect[J]. Nanomedicine : nanotechnology, biology, and medicine, 2018, 13(4): 391-405. [128] ZHANG M, CHENG J, LUO J, et al. Protective effects of Scutellariae Radix Carbonisata-derived carbon dots on blood-heat and hemorrhage rats[J]. Frontiers in Pharmacology, 2023, 14: 1118550. doi: 10.3389/fphar.2023.1118550 [129] ALTINTIG E, SARıCı B, KARATAŞ S. Prepared activated carbon from hazelnut shell where coated nanocomposite with Ag+ used for antibacterial and adsorption properties[J]. Environmental Science and Pollution Research, 2022, 30(5): 13671-13687. doi: 10.1007/s11356-022-23004-w [130] CHENG P, XUE X, SU J, et al. (1)H NMR-based metabonomic revealed protective effect of Moutan Cortex charcoal on blood-heat and hemorrhage rats[J]. J Pharm Biomed Anal, 2019, 169: 151-158. doi: 10.1016/j.jpba.2019.02.044 [131] YUE Z, XIAOLI G, JUAN Z, et al. Effect of the oxygenic groups on activated carbon on its hemocompatibility[J]. Colloids and surfaces B, Biointerfaces, 2024, 233: 113655. doi: 10.1016/j.colsurfb.2023.113655 [132] WANG S, ZHANG Y, SHI Y, et al. Rhubarb charcoal-crosslinked chitosan/silk fibroin sponge scaffold with efficient hemostasis, inflammation, and angiogenesis for promoting diabetic wound healing[J]. Int J Biol Macromol, 2023, 253(Pt 2): 126796. -

 点击查看大图
点击查看大图
计量
- 文章访问数: 47
- HTML全文浏览量: 25
- 被引次数: 0




 下载:
下载:





